“From a diagnostic standpoint, particularly in diseases of the brain and spine, imaging is everything,” says Dr. Anthony Asher, President of Atrium Health Neurosciences Institute. Every day, neurosurgeons like Asher, rely on advanced imaging to better understand numerous complex diseases along with their relationship to intricate structures in the brain and other parts of the nervous system.
Atrium Health’s new intraoperative MRI (iMRI) technology puts the hospital system on the forefront of advanced imaging, becoming the first hospital in the region to obtain and apply such technology. With iMRI, neurosurgeons practicing at Atrium Health Carolinas Medical Center will be able to operate with real time, gather information from more accurate images and access these images more efficiently.
“At Atrium Health, we don't just chase expensive technologies for the sake of novelty or a because of a blind allegiance to ‘innovation’’’, says Asher. “We have a strong commitment to responsible resource use; in that regard, we obtain technologies that can really make a difference in patient’s lives”.
With iMRI in their toolbox, Asher and his colleagues are excited to make exactly that type of patient-focused impact.
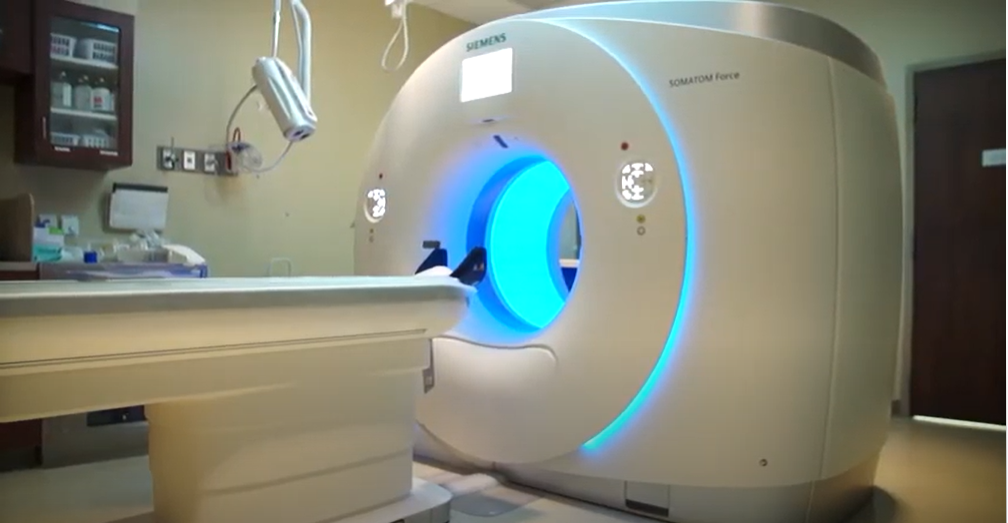
The MRI: A revolutionary tool
Imaging has always been a crucial tool for diagnostic medicine — but it was only in the past few decades that technology started to exponentially advance. First came the CT scan, which was a significant advancement over crude X-ray technology. Then, less than a decade later came a massive game-changer in the world of imaging: magnetic resonance imaging, or MRI.
“From the standpoint of improving our diagnostic and decision making capabilities, advances in MRI technologies have created explosive growth in our ability to understand various things about the brain, whether it's brain activity in real time, nuances about complex pathologies, or connections within neural networks” says Asher.
“From the standpoint of treatment, these advanced imaging technologies when combined with other surgical tools such as image-based navigation, provide us with a number of essential capabilities. First and foremost being the ability to achieve millimeter accuracy when plotting surgical trajectories in and around the brain. For example, we can literally point at the surface of the skull and know exactly where the lesion is relevant to that surface anatomy — and then make very precise openings and precise approaches to various lesions in the brain.”
Throughout surgery, a neurosurgeon will refer to these images of the patient’s brain — typically obtained before surgery — to guide their work. But inevitably the brain’s position will change during surgery, and the pre-operative image they had used at the beginning of a procedure inevitably becomes less accurate as a case progresses. In the past, such “brain shift” sometimes necessitated ending a surgery, obtaining another MRI, then initiating a second procedure at another time. Although that process was an advance over previous techniques, it wasn’t very efficient, and it required exposure of patients to an additional anesthesia. Avoidance of such scenarios is just one reason why iMRI technology is so transformative.
The unique power of iMRI
What the iMRI enables neurosurgeons to do is image the patient after a certain portion of the procedure, essentially in real time. While the patient is still under anesthesia, the surgical team can wheel the patient over to the iMRI and generate images without having to wake up the patient.
“Let's say our eyes, even with the assistance of a high-powered surgical microscope, just couldn't perceive a certain portion of a deeply seated brain tumor,” says Asher. “With iMRI, we can safely take another image of the brain, determine the relationship of residual tumor to the areas we have already operated in, and perform a more complete, not to mention safe, surgical procedure. An added benefit, of course, is that the patient can avoid another anesthesia.”
During neurosurgery, the brain is bound to move due to the release of spinal fluid. It’s possible in some circumstances that parts of the brain anatomy might shift up to a few centimeters, making it harder to accurately assess the exact location of various pathologies to normal brain structures. That’s a prime reason why it’s so important for neurosurgeons to have updated images of the brain throughout surgery.
“In circumstances where there's been a lot of brain shift, the iMRI is a tremendously powerful technique, because we can see the brain in its most up-to-date state,” explains Asher. “Now with much more confidence, even if the brain has shifted a couple of centimeters, we can accomplish our objectives. It's a really phenomenal capability in that regard.”
New surgical horizons
Working from accurate imagery is all the more vital when dealing with tumors that might be deep in the brain, such as gliomas. This common type of brain tumor arises from tissue within the brain. These tumors can often be large and can either displace or even invade brain regions responsible for essential activities. Tumor removal alone can cause substantial shift in the overall position of the brain during surgery. This creates challenges if a surgeon has to rely solely on images obtained before a surgical procedure begins.
“If we don't have almost perfect spatial accuracy when we’re operating on these deep tumors, we can really find ourselves in a difficult situation with respect to achieving complete and safe removal,” says Asher. “That’s particularly the case if these tumors are next to or invade what we call ‘eloquent structures’, which directly control essential functions such as speech or movement. We absolutely need to know where we are relative to those structures, preferably in real time”
iMRI enables neurosurgeons to precisely visualize brain regions and appreciate their three-dimensional characteristics accurately throughout these advanced surgeries. They can understand where tumors and other pathologies are relative to these essential connection systems in the brain — and avoid them.
“Going forward, I suspect many areas of brain surgery will be significantly transformed by iMRI. In the case of functional neurosurgery, being able to see in real time where we are making lesions to treat conditions such as epilepsy with millimeter accuracy will be a tremendous advantage,” says Asher. “For example, we can make sure that the lesion is exactly where it is supposed to be before the patient leaves the operating room.”
Putting Atrium Health ahead of the curve
Asher estimates that at this point only about 80 hospitals in the country have iMRI technology, though that number is sure to grow over the coming years. Adopting this technology after its efficacy has been established but still early in its overall adoption by the broader medical community aligns with Atrium Health’s forward-thinking culture and willingness to engage with innovative techniques.
And behind every great technology is a team of people that enables it to perform at the highest level. A great deal of coordination on the part of the Atrium Health medical staff goes into ensuring the iMRI technology is used safely and effectively.
“It’s really a fantastic example of teamwork, coordination, standardization of procedures, all making sure we're keeping the patients safe and doing the right thing,” says Asher. “The technology is remarkable, but I think that what we do as a team is equally remarkable.”
“At the end of the day, Atrium Health is committed to the intelligent acquisition of technologies that can change patients' lives and improve the safety of care and improve our ability to promote wellbeing,” says Asher. “Once a technology has been appropriately vetted, we put it through a process and if there's a consensus that this is what we need to provide the highest level of care in a quaternary center, we go out and get it.”