Some patients battling treatment-resistant depression or other mood disorders may get to a point where they feel like they’re out of options. They may have tried several medications and/or months of talk therapy with little relief from their symptoms. Other patients with depression may have trouble taking medications due to severe side effects.
For example, Robert, a 79-year-old patient from Charlotte, has dealt with depression for most of his life. In 2021, his medication stopped working, putting him into severe depression. His mental health got so bad that he described himself as being in a “nonfunctional state.”
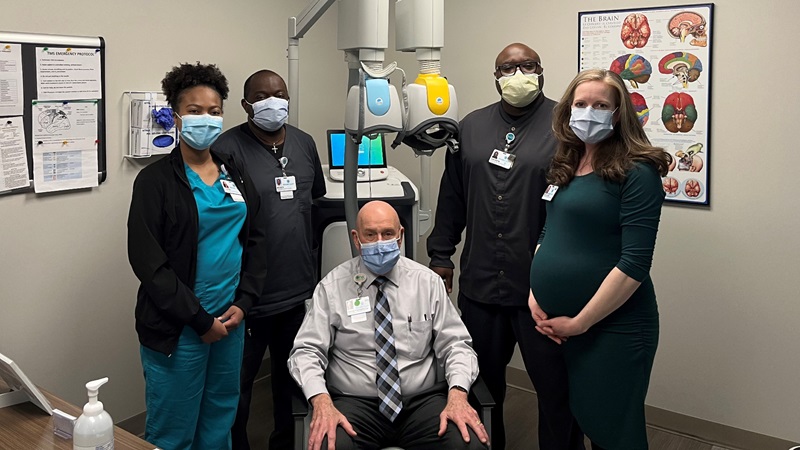
Things started to improve for Robert after he completed a series of transcranial magnetic stimulation (TMS) treatments at Atrium Health Behavioral Health Interventional and Neurocognitive Psychiatry (INP). These experts are giving patients like Robert hope – with more treatment options for severe depression and other mood disorders.
TMS is a neuromodulation treatment that delivers brief, magnetic pulses to regions of the brain that can affect mood. The FDA has approved TMS to treat severe depression, depression with anxiety and obsessive-compulsive disorder. Specific TMS devices have also been approved to help patients with smoking cessation. While TMS can be helpful in treating bipolar depression, it has not yet been approved by the FDA for this condition.
Why should patients consider this innovative therapy? “One of the most exciting things about this treatment is that it causes no side effects for most patients,” explained Dr. Ervin Thompson, interventional psychiatrist with Atrium Health Behavioral Health Services. “In rare cases, patients may get headaches. Other side effects may include scalp discomfort at the treatment site and tingling or spasms in the face muscles.”
TMS has helped many patients battling treatment-resistant depression. “It has a 50-60% response rate for severe depression,” said Dr. Nicole Aho, interventional psychiatrist with Atrium Health Behavioral Health Services.
What to expect
During this noninvasive procedure, the patient is seated in a comfortable chair and given earplugs to wear. An electromagnetic coil is placed against the patient’s scalp near their forehead. The coil delivers magnetic pulses that stimulate nerve cells in the region of the brain involved in controlling mood and depression. The patient hears clicking sounds and feels tapping on their forehead during treatment.
TMS is available as daily treatments Monday through Friday for six weeks. Depending on the selected protocol, TMS sessions can last from three to 45 minutes. Since there’s no anesthesia involved, patients can return to normal activities right after TMS treatment. This means they’re able to drive themselves to and from treatment sessions.
Robert had 28 TMS treatments over the course of five weeks. He described the TMS therapy room as “very comfortable.” And he gave the TMS team five stars for their bedside manner and expertise.
According to Dr. Aho, most patients start to notice benefits within four weeks of treatment. A study published by The Journal of Clinical Psychiatry revealed that about two-thirds of patients were still well 12 months after treatment when they continued adjunctive care, like medication and therapy.
“Since TMS is not considered a cure or designed to fully take the place of medication or talk therapy, we strongly encourage patients to continue taking their medications as directed,” said Dr. Aho. “While ongoing therapy is not required for TMS patients, they usually benefit from retreatment if needed."
Comprehensive, personalized treatment
Atrium Health Behavioral Health INP offers the most comprehensive interventional psychiatry program in the region. Its dedicated team of board-certified physicians, registered nurses and certified technicians uses a variety of devices and protocols to treat depression and other mood disorders in a progressive manner.
The TMS team takes the time to discuss all possible treatment options and works with each patient to determine the best neuromodulation treatment to meet their needs.
During the consultation, the doctor reviews the patient’s full health history, discusses all medications they’ve tried and considers comorbidities (coexisting conditions) that could affect treatment.
“Our goal is to improve health, elevate hope and advance healing for all behavioral health patients using a variety of neuromodulation treatments,” Dr. Aho said. “Thanks to our diverse expertise, we have the flexibility to offer other treatment methods to help patients who don’t respond to TMS.”
Leading-edge protocols and devices
Among the available TMS protocols, Theta Burst Technology delivers rapid treatment, reducing treatment time from 19 minutes to just three minutes per session. “Since patients can be in and out of treatment so quickly, this protocol is less disruptive and more convenient for those with busy schedules,” explained Dr. Aho.
The TMS team can deliver TMS therapy using two different coils. The figure-8 coil allows the team to provide rapid TMS treatments for depression. The H coil allows the technician to apply the treatment deeper into the brain, a technique known as deep TMS. The team has specialized H coils to treat depression, depression with anxiety and obsessive-compulsive disorder. They also recently ordered a new H coil to help patients with smoking cessation. They plan to offer this treatment soon to treat general depression as well as depression with anxious features.
History of safety and advanced training
Atrium Health has a long history of providing neuromodulation treatments to thousands of patients safely and effectively. The hospital has offered TMS therapy since 2012.
Atrium Health Behavioral Health INP clinicians have extensive experience in treating mood disorders. They have also had in-depth, hands-on training in the use of TMS from nationally renowned physicians who first pioneered the technology.
“To ensure your safety, our team has taken specialized certification courses in TMS,” Dr. Aho said. “Plus, most of our teammates and technicians are members of the Clinical TMS Society, which helps us stay up to date on the latest research and the most cutting-edge protocols and therapies available.”
While a technician administers TMS therapy, there’s a doctor next door to the TMS therapy room in case the patient has questions, needs a coil adjustment or experiences a medical emergency. Many medical centers only require a doctor to be “readily available” but may not require them to be on-site at the facility.
Robert felt safe during treatment as he was closely monitored at all times. “Other facilities had two technicians monitoring six patients at once during treatment,” he noted. “That’s why I didn’t want to go anywhere but Atrium Health. I knew I would get the personalized attention I needed.”
Research and education
Researchers with Atrium Health Behavioral Health INP are working to collaborate with Atrium Health Wake Forest Baptist in order to expand their research efforts and improve patient care. Future studies may be used to explore ways to use TMS to treat substance use disorders and sleep disorders.
Researchers at Stanford University are studying a potentially faster TMS protocol. Instead of the standard six-week treatment schedule, this protocol only requires 10 sessions per day over a five-day period (50 total sessions). Initial results show an 86% response rate to the treatment. In the future, this rapid treatment could be used to help patients with mental health conditions in the emergency department or during inpatient mental health hospitalizations.
Patients benefit from Atrium Health Behavioral Health INP’s rich academic culture. “With so many students and residents rotating through our clinic, we’re always learning as an organization,” Dr. Aho explained. “That helps keep us on our toes. We’re constantly researching questions and keeping up to date on the latest literature. We’re learning from them, and they’re learning from us. We’re training the next generation of interventional psychiatrists.”
Better health and relationships
How’s Robert doing now? “I’m great!” he said. “It has changed my life. My interpersonal relationships have improved. People like being around me a lot more, and I enjoy being around them.”
He added, “Atrium Health offers great mental health services. If you’re struggling, go see them.”
Learn more
To learn more, visit Atrium Health Behavioral Health INP or call 704-512-7578.



