Each year, more patients are hospitalized for osteoporosis-related fractures than for breast cancer, stroke and heart disease combined. But why are there so many hospitalizations?
“Osteoporosis is an underdiagnosed, undertreated disease that causes the bones to become weak or brittle,” explains Anne Lake, doctor of nursing practice with Atrium Health Wake Forest Baptist’s Fracture PreventionProgram, certified orthopaedic nurse practitioner and clinical densitometrist. “Many people don’t realize they have it until they develop symptoms of advanced disease, including fractures, height loss, back pain and poor posture.”
Annually, osteoporosis affects up to 37 million people worldwide over 55. If left untreated, this chronic condition often leads to a loss of independence and decreased quality of life. The financial burden of osteoporosis is over $95 million each year, which includes the cost of fracture treatment and long-term disease management.
Atrium Health’s Fracture Prevention Program experts are focused on educating patients about osteoporosisand identifying it at its earliest stages. Their goal is to implement fracture prevention strategies that reduce or eliminate the disease’s debilitating effects and enhance quality of life.
Atrium Health’s Fracture Prevention Program has grown into a nationally recognized initiative, originally launched by Lake at Atrium Health Wake Forest Baptist in 2013 (prior to its integration with Atrium Health). Two years ago, she partnered with JoAnn Holzinger, family nurse practitioner with Atrium Health Orthopaedics Surgery, a facility of Atrium Health Carolinas Medical Center, to start a Fracture Prevention Program at Carolinas Medical Center.
Bone health and aging
Some people may think that osteoporosis is caused by a lack of exercise or nutrients. In reality, the condition is an age-related process that changes the body’s bone-related metabolism.
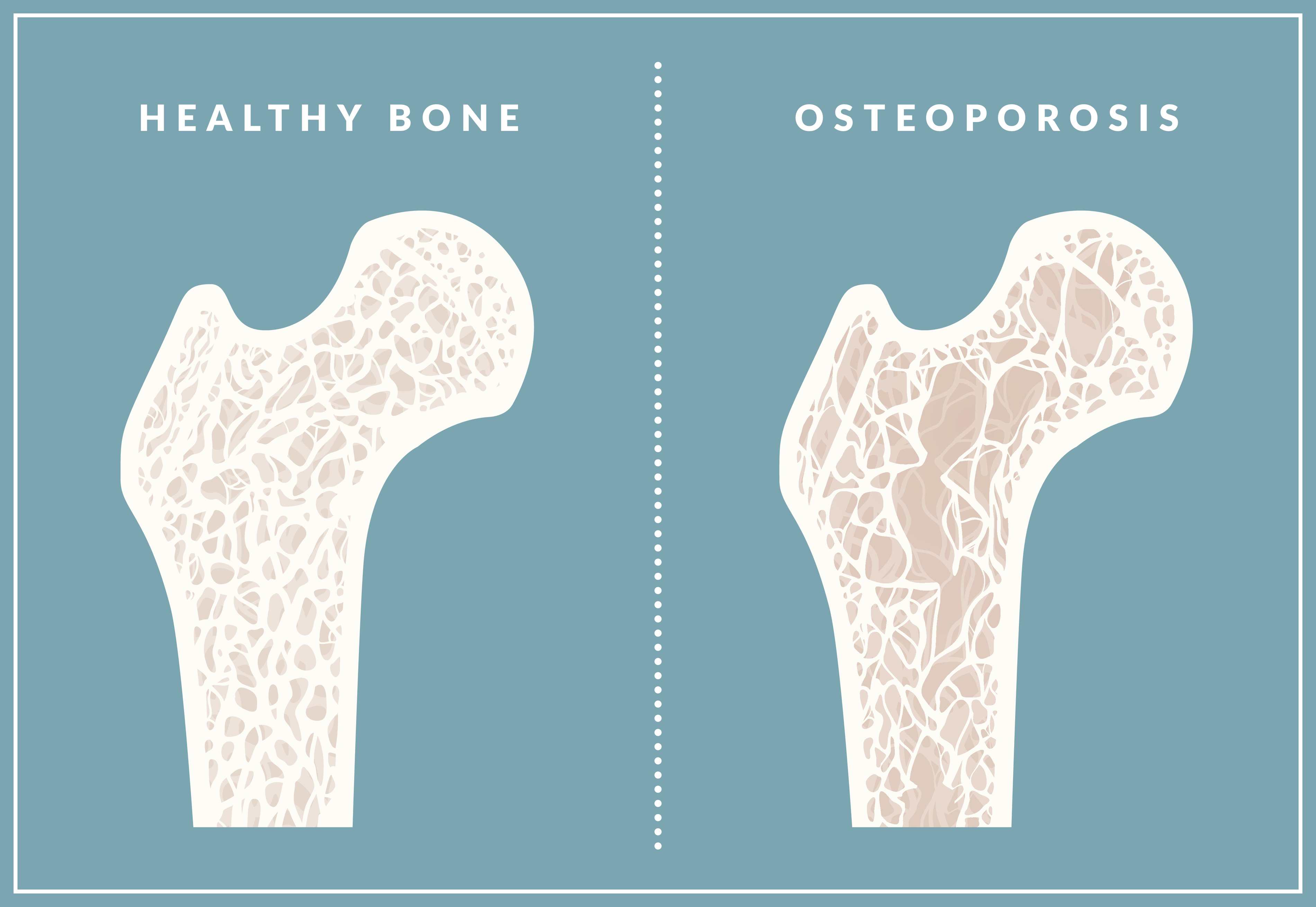
“Our bone is alive and has a constant bone-building and removal process going on inside,” explains Holzinger. “After age 50, we lose more bone than we make each year, causing the inside of the bone to become more hollow. When we fall, we may fracture because our bone becomes more like an English muffin, full of nooks and crannies.”
As people age, many are prescribed medications that block the absorption of nutrients that bones need to grow, including calcium and vitamin D. For example, these medications are known to interfere with nutrient absorption:
- Acid reflux medications, such as proton pump inhibitors
- Depression and anxiety medications, such as selective serotonin reuptake inhibitors
- Anti-inflammatory medications for rheumatoid arthritis, such as prednisone
“The aging population is living longer than they used to,” notes Lake. “Our goal is to help you maintain an active, independent lifestyle as long as possible.”
Patients most at risk
While everyone will eventually have bone loss due to aging, patients with the following characteristics or history are most at risk for developing osteoporosis:
- Women age 65 and older
- Men age 70 and older
- Men with low testosterone
- Individuals with:
- Short stature
- Low BMI
- A history of eating disorders or gastric bypass
- A history of cancer treatment involving radiation or chemotherapy
- A history of immunosuppressants for autoimmune disease or transplant
Evaluating bone health
“You can see your skin aging, but you can’t see your bones aging,” Lake says. “So you may not notice the symptoms of osteoporosis until your bones begin to fracture.”
According to Lake, women tend to lose bone very quickly during the first five years of menopause. Starting in their early 50s, these patients are losing bone faster than their bodies can replace it. She recommends screening these women within the first one to two years of menopause.
When it comes to screening for bone strength, bone health experts are interested in measuring bone density (thickness or thinness of bone from mineralization) and bone quality (microarchitecture of the bone), both of which diminish with age. In addition, blood tests are used to measure bone health, bone quality, bone formation and bone turnover.
Measuring bone density
A dual-energy X-ray absorptiometry (DEXA) scan is a low-dose X-ray that measures the minerals in bones to determine bone density.
“For many patients, health insurance plans will cover a DEXA scan every two years,” says Holzinger. “It provides important information about bone health and the effectiveness of treatment. It’s just as important as a mammogram.”
A DEXA scan may reveal osteopenia, which indicates a loss of bone density. Patients with osteopenia are at an increased risk of bone fractures and may progress to osteoporosis if left untreated.
Measuring bone quality
Trabecular bone score (TBS) has become the gold standard for assessing bone health when used alongside traditional bone density testing. A relatively new diagnostic tool, TBS enhances conventional bone density measurements by evaluating the microarchitecture of bone, offering a more comprehensive view of fracture risk. Specifically, TBS assesses the structure of trabecular (spongy) bone, which is located at the ends of long bones and in the spine. A higher TBS score indicates better bone quality.
Several Atrium Health Wake Forest Baptist locations offer TBS along with bone density testing to give doctors a clearer picture of total bone strength.
Key advantages of TBS:
- Fracture risk indicator. TBS predicts fracture risk independently of bone mineral density, identifying individuals at risk who might not be detected by bone density testing alone.
- Noninvasive technique. TBS is derived from standard DEXA scans, making it a noninvasive and convenient method for clinicians to assess bone health.
- Tailored treatment interventions. By providing additional insights into bone quality, TBS helps clinicians tailor treatment plans more effectively, ensuring patients receive personalized care.
Fragility fractures
Unfortunately, many patients are not diagnosed with osteoporosis until after they have a fragile bone fracture (a fall from standing height). While treating fragility fractures is essential, addressing the underlying cause is just as important.
“A fragility fracture is a teaching moment in orthopedics,” Holzinger explains. “It’s an ideal time to evaluate the patient’s bone density, teach them bone-building habits and offer them medication to stabilize or reverse their bone loss.”
Fracture prevention strategies
Atrium Health bone experts use two pathways to prevent fractures in patients with bone loss:
- Slow bone loss and reduce the risk of fracture
- Rebuild bone and reduce the risk of fracture
“All recommended treatments aim to reduce your fracture risk,” says Lake. “While improving bone density is a goal, the primary focus is on preventing future fractures. Even if your bone density stays the same, avoiding fractures is still considered a success.”
Here are some ways to optimize your bone health:
-
Exercise. Weight-bearing exercise and strength training help build coordination and slow bone loss.
-
Nutrition. Bones require proper nutrients and minerals to stay strong. A Mediterranean diet – rich in vegetables, legumes, fruits, nuts and olive oil – can help support bone health. The diet includes a moderate amount of fish.
-
Supplements. Vitamin D and calcium supplements are recommended if these are lacking in your diet.
-
Medication. Patients who have had a fragility fracture or an osteoporosis diagnosis should consider taking medication to reduce their risk of fracture. Many of these medications work by slowing down the cells that resorb (break down) bone, giving bone-building cells more time to build. Other anabolic medications, which patients administer by injection, turn on the body’s bone-building cells.
- Balance training. This type of physical therapy focuses on building strength and improving balance. Carolinas Medical Center’s Better Balance Program features personalized therapy and patient education to reduce the risk of falling. Participants receive home safety tips and footwear recommendations.
Easy access to care
Atrium Health Wake Forest Baptist has seven satellite locations for treating patients with bone health issues. Carolinas Medical Center has three satellite locations in downtown Charlotte and the surrounding region. Bone health experts are expanding the program to other Atrium Health locations in Georgia, Advocate Health locations in Illinois and Advocate Aurora locations in Wisconsin.
This year, the program is focused on providing easy access to the care and resources patients need to live well and stay well.
“We believe that every patient being treated for a fragility fracture deserves the same level of fracture care,” explains Lake. “Our team will fix the fracture and work to prevent future fractures. If we’re treating the first fracture, we want it to be the last fracture.”
Education and patient-centered care
Atrium Health’s Fracture Prevention Program experts are educating patients, resident physicians and orthopedic surgeons on the value of addressing the underlying causes of fragility fractures.
Both Lake and Holzinger have processes in place to help patients with bone health issues. Once a patient is admitted at Atrium Health Wake Forest Baptist with a hip fracture, they are automatically referred to the Fracture Prevention Program. Holzinger regularly visits Atrium Health facilities in Charlotte and reviews admitted patients. She recommends the Fracture Prevention Program for those who have experienced fragility fractures and explains how to obtain a referral to an orthopedic specialist.
“We want to motivate patients to ask their orthopedic providers about strategies to prevent future fractures,” Holzinger notes.
Lake and Holzinger are educating nurses, resident doctors and attending physicians about fragility fractures to ensure that bone health is not forgotten. They also provide access to the resources needed to help patients optimize their bone health.
“Our program provides a coordinated care model that includes all teammates along the continuum of care,” Lake says. “Ideally, we prefer that the orthopedist takes the lead in identifying at-risk patients, but we also have support from our physical therapists, pharmacists, primary care physicians and resident doctors.”
The Fracture Prevention Program is helping patients achieve the best possible outcomes for bone health.
“We aim for patients to have strong, healthy bones for life,” says Holzinger. “Our goal is to help them maintain independence and achieve their longevity goals. We’re committed to optimizing their long-term health.”
To make an appointment with either Fracture Prevention Program, call 336-716-8735.



