Researchers Receive $30 Million Award to Study Novel Rehab Program for Heart Failure Patients
Scientists will test a potential new treatment for older patients with heart failure with preserved ejection fraction (HFpEF)
WINSTON-SALEM, N.C. – Oct. 6, 2022 – The National Institute of Aging (NIA), part of the National Institutes of Health, recently awarded Wake Forest University School of Medicine a five-year grant expected to total $30 million to support research to test a novel rehabilitation program designed for older patients hospitalized for acute heart failure.
Heart failure, a condition in which the heart is not pumping blood and oxygen efficiently, affects more than 6 million adults in the U.S. and is the leading cause of hospitalization among older persons.
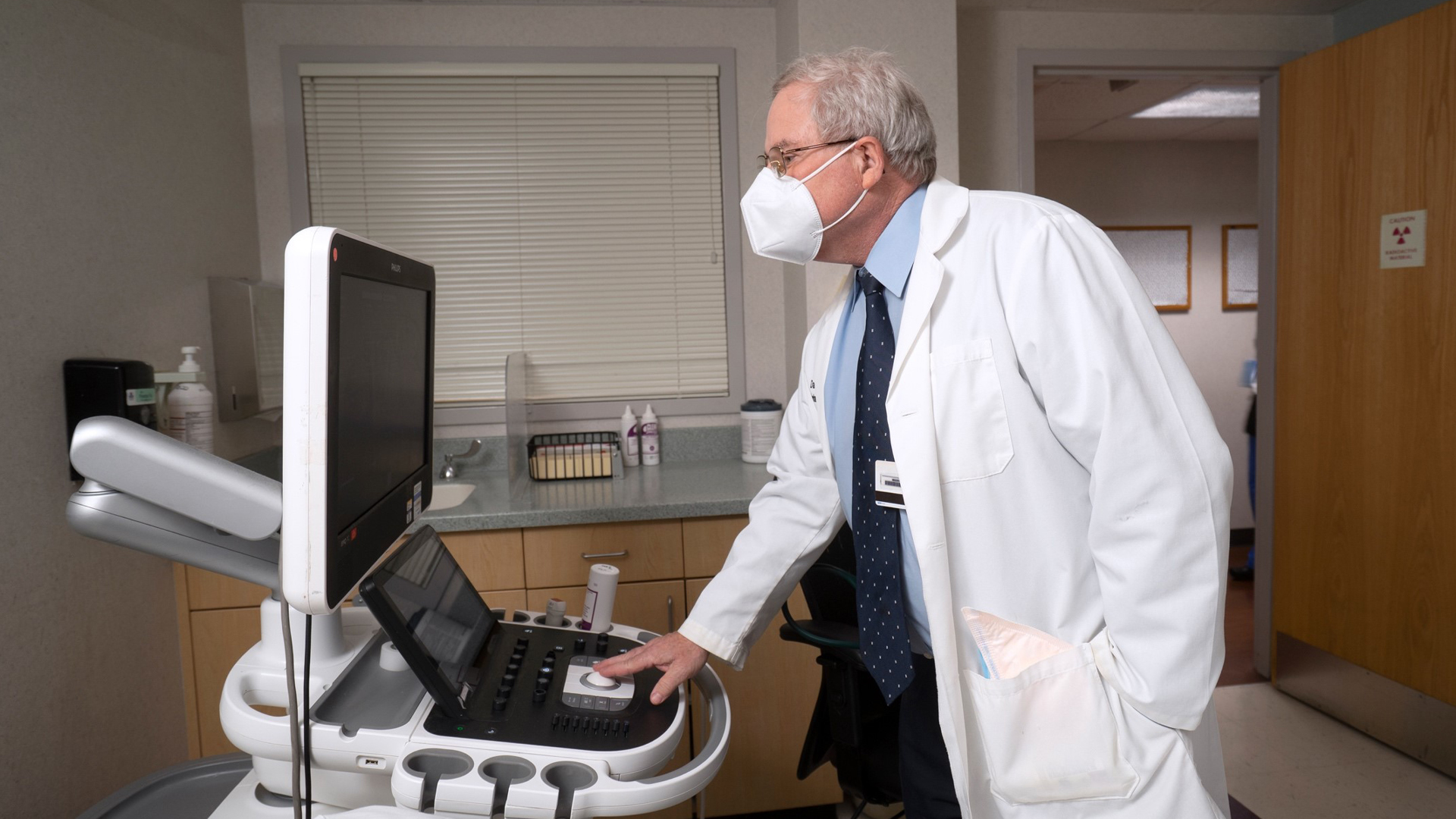
Led by Dr. Dalane Kitzman, professor of cardiovascular medicine at Wake Forest University School of Medicine, a team of scientists from Wake Forest, Duke University, Thomas Jefferson University and partner institutions will lead a Phase III REHAB-HFpEF trial to examine whether a novel physical rehabilitation intervention will reduce rehospitalizations and mortality in patients hospitalized for heart failure with preserved ejection fraction (HFpEF). Ejection fraction refers to the contraction ability of the heart.
HFpEF is the most common form of heart failure in older persons. Unfortunately, these frail patients have poor outcomes, and there are few proven treatments available.
“Our previous research, published last year in the New England Journal of Medicine, showed that our novel intervention significantly improves physical function in these patients,” Kitzman said. “We hope a larger trial will show that the intervention also reduces the likelihood of repeat hospitalization and death.”
The REHAB-HF program was developed by a team of physical rehabilitation experts specifically for an older, frail adult population who have very poor physical function due to aging and chronic heart failure. Kitzman said these patients’ physical function is exacerbated by their hospital experience and bedrest, and the severe deficits often persist long after discharge, and without specialized help, patients often never recover fully.
The intervention program, which is individually tailored, involves strength, balance, endurance and mobility training exercises. The program is implemented as early in the hospital stay as possible and transitions to an outpatient facility for three sessions a week for 12 weeks and then continues with exercise at home.
In the previous study, researchers found that hospitalized older patients with acute heart failure had significant gains in physical function, including balance, mobility, strength, endurance and in quality of life, compared with those receiving usual care. But the number of participants was too small to determine if the intervention also improved the important outcomes of frequent rehospitalization and death.
Importantly, the benefit appeared to be greatest in patients who had HFpEF. This larger study will focus on this important subgroup of patients, who were also the frailest and had the most severe disability.
“We are targeting an important unmet need in one of the largest, most vulnerable and underserved populations,” Kitzman said. “These patients with acute HFpEF don’t have many treatment options because most treatments previously tested have not been effective. These results could change clinical practice and improve the health of this high-risk population.”
The trial includes 20 sites across the country including Atrium Health Wake Forest Baptist Medical Center, in Winston-Salem, and Atrium Health Sanger Heart & Vascular Institute, in Charlotte. Recruitment is expected to begin in early 2023.
This research is supported by NIA grant R01AG078153. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
